Osteonecrosis of the Humeral Head
|
||||||
Introduction
Physiotherapy in Edmonton for Shoulder Issues
Welcome to In Step Physical Therapy's resource about Osteonecrosis of the Humeral Head.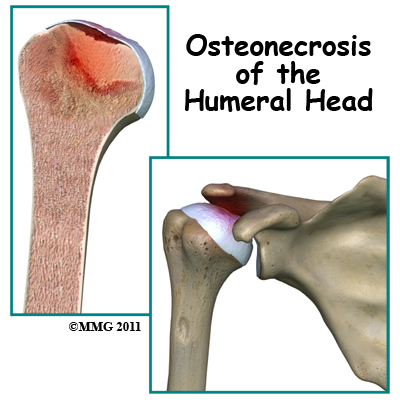 Osteonecrosis of the humeral head is a condition where a portion of the bone of the humeral head (the top of the humerus or upper arm bone) loses its blood supply, dies and collapses. Another term used for osteonecrosis is avascular necrosis. The term avascular means that a loss of blood supply to the area is the cause of the problem and necrosis means death.
Osteonecrosis of the humeral head is a condition where a portion of the bone of the humeral head (the top of the humerus or upper arm bone) loses its blood supply, dies and collapses. Another term used for osteonecrosis is avascular necrosis. The term avascular means that a loss of blood supply to the area is the cause of the problem and necrosis means death.
This condition has been reported in all age groups but seems more common between the ages of 20 and 50. Men are affected by osteonecrosis of the shoulder twice as often as women but women with osteonecrosis from an autoimmune disease (e.g. lupus) develop this condition more often than men with the same disease.
This guide will help you understand:
- how osteonecrosis develops
- how health care professionals diagnose the condition
- what treatment options are available
- what In Step Physical Therapy’s approach to rehabilitation is
#testimonialslist|kind:all|display:slider|orderby:type|filter_utags_names:Shoulder Pain|limit:15|heading:Hear from some of our patients who we treated for *Shoulder Pain*#
Anatomy
Where does this condition occur?
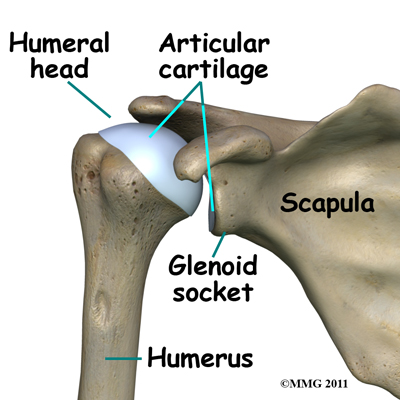
The shoulder joint is a ball-and-socket joint. The ball portion of the joint is called the humeral head. The humeral head is the uppermost part of the humerus, or upper arm bone. The shoulder socket is called the glenoid fossa. This socket is shallow and is part of the scapula (shoulder blade). The surface of the humeral head and the inside of the fossa are covered with articular cartilage. Articular cartilage is a tough, slick material that allows the surfaces to slide against one another with very little friction. The cartilage is about one-quarter of an inch thick in most large weight-bearing joints, but a bit thinner in the shoulder, which generally doesn't support much weight.
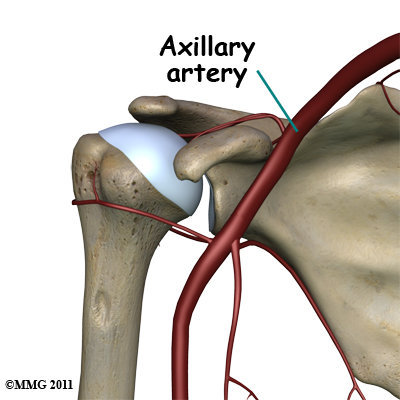
Large blood vessels supply the arm with blood. The large axillary artery travels through the axilla (armpit). If you place your hand in your armpit, you may be able to feel the pulsing of this large artery. The axillary artery has many smaller branches that supply blood to different parts of the shoulder. The shoulder has a very rich blood supply, but unfortunately if this blood supply is damaged, there is no backup.
Related Document: In Step Physical Therapy's Guide to Shoulder Anatomy
Causes
What causes this condition?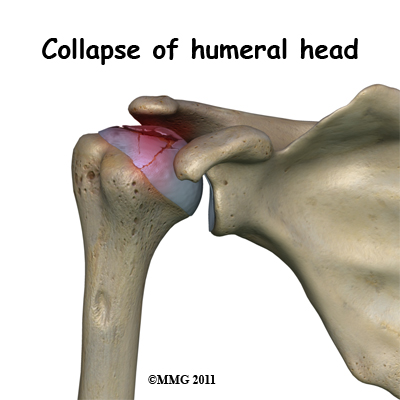 Bone tissue is constantly being remodeled which means that old bone is removed and replaced with new bone. Osteonecrosis occurs when there is a loss of blood circulation in the bone of the humeral head. This causes the cells that remove and produce new bone to die in the area of lost circulation. New bone is no longer produced, but the old bone matrix still survives. Without the constant ability to repair itself through remodeling, the dead bone matrix eventually begins to lose strength and crumble. This causes the bone matrix to collapse. New blood vessels begin to grow into the area, but this is a slow process. The situation becomes a race to see whether new blood vessels will grow into the area and restore the ability to remodel the bone or whether bone collapse will occur.
Bone tissue is constantly being remodeled which means that old bone is removed and replaced with new bone. Osteonecrosis occurs when there is a loss of blood circulation in the bone of the humeral head. This causes the cells that remove and produce new bone to die in the area of lost circulation. New bone is no longer produced, but the old bone matrix still survives. Without the constant ability to repair itself through remodeling, the dead bone matrix eventually begins to lose strength and crumble. This causes the bone matrix to collapse. New blood vessels begin to grow into the area, but this is a slow process. The situation becomes a race to see whether new blood vessels will grow into the area and restore the ability to remodel the bone or whether bone collapse will occur.
The articular cartilage on the surface of the humeral head does not rely on the blood supply of the bone to survive. The articular surface is nourished by something called synovial fluid, which is within the joint, therefore the articular cartilage survives the loss of blood flow to the bone. The articular cartilage, however, relies on the bone underneath to keep its round shape. When the bone underneath collapses, the articular cartilage loses its round shape and no longer fits, or matches, the shape of the glenoid socket. The top of the humeral head (the ball portion) collapses and begins to flatten. The constant abnormal friction between the two mismatched joint surfaces causes mechanical wear and tear in both the humeral head and the glenoid socket, similar to two pieces of a mismatched piece of machinery. Due to this friction the joint begins to wear itself out. This degeneration is called osteoarthritis.
There are two forms of humeral head osteonecrosis: traumatic and atraumatic. The traumatic type can develop after an injury such as a bone fracture or shoulder dislocation. The atraumatic form occurs with the use of corticosteroids, or it can be associated with other diseases or blood disorders (e.g., sickle cell disease, problems with coagulation or making blood clots). Sometimes it develops with no known cause. In those cases, it is termed idiopathic osteonecrosis (unknown cause).
There does seem to be a genetic link to developing osteonecrosis but exposure to certain risk factors is also part of the picture. For example, alcohol abuse, tobacco use, chemotherapy, radiation, pregnancy, inflammatory bowel disease, and organ transplantation are all considered associated risk factors. A clear link exists between osteonecrosis and alcoholism. Although the exact process is not known, excessive alcohol intake somehow damages the blood vessels and leads to osteonecrosis.
Another population at increased risk of developing osteonecrosis is organ recipients. Organ recipient patients must be on lifelong steroids to prevent inflammation, infection, and rejection of the organ. Unfortunately, these medications have the adverse side effect of endangering blood supply and weakening the bone.
Symptoms
What does osteonecrosis feel like?
The first symptom of osteonecrosis of the humeral head is shoulder and arm pain. The location of the pain is difficult to isolate. You may not be able to point to it with one finger. You may feel like the pain is deep and throbbing. You may have difficulty reaching your arms out to the sides or overhead.
At first, the symptoms seem to come and go, but as the problem progresses the symptoms become more constant and stiffness develops in the shoulder joint. Pain may radiate, or travel, from your shoulder down to your elbow. There may be a sound and sensation of crunching in the joint (called crepitus) and the joint may feel like it locks. With subsequent arthritic changes in the joint, range of motion decreases. Eventually, the pain will also be present at rest and may even interfere with sleep. In a small number of cases, there are no symptoms despite X-rays that show advanced disease.
Diagnosis
How do health care professionals diagnose this condition?
Your health care professional will conduct a thorough history and carry out a clinical exam. The history helps identify associated risk factors, which will have to be addressed during treatment in order to get the most successful results. Your health care professional will inquire about when the pain started and if it occurred due to an injury or whether it came on gradually. They will also ask you about what makes the pain better or worse, and if you feel that the pain is getting worse overall or staying the same. Your health care professional will also check other joints for any signs of similar problems. In about half the patients, osteonecrosis is also present at the hip, knee, ankle, wrist, and/or elbow.
Lab studies can be done to rule out infection or test for systemic diseases or blood disorders that can cause osteonecrosis.
Standard X-rays are usually ordered to confirm the diagnosis. Several different views are needed. Besides the usual anterior-posterior (AP) views, radiographs should include views with the joint in external (outward) and internal (inward) rotation. These added X-ray views will help show all areas of the diseased humeral head, which is important information for planning treatment.
X-rays don't always show all of the changes until the condition has been present for quite some time. MRIs may be used to define more clearly early changes in fat and water content of the bone marrow that won't be seen on X-ray. Bone scans have fallen out of favor for the detection and diagnosis of osteonecrosis as studies show that only one-third of true cases are successfully identified with this imaging tool.
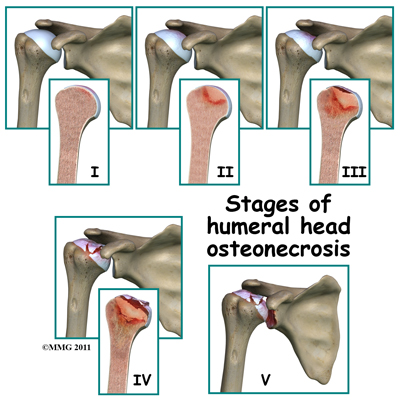
Treatment is based on the severity of disease, so part of the diagnosis is to identify what stage the disease is in. The stages range from stage I-V. In stage I no changes are seen on X-ray images. In stage V (the most advanced disease) the humeral head is collapsed and the socket is damaged as well. There may also be soft tissue tears present in the more advanced stages.
Treatment
What treatment options are available?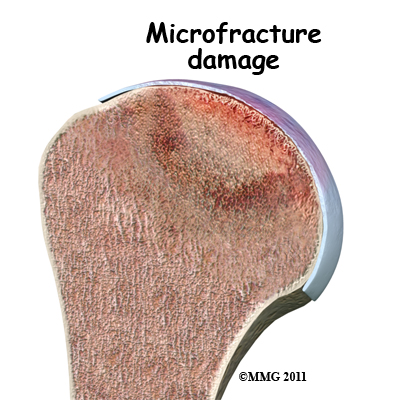 The first goal in treating osteonecrosis of the humeral head is to save the bone. Left untreated, the disease process will continue until the layer of bone just under the joint surface cracks causing small microfractures.
The first goal in treating osteonecrosis of the humeral head is to save the bone. Left untreated, the disease process will continue until the layer of bone just under the joint surface cracks causing small microfractures.
Once enough microfactures occur, the bone begins to collapse and the articular cartilage covering the joint surface also starts to collapse. Eventually, there will be damage to the entire shoulder joint.
The second goal is to keep the shoulder functional while relieving pain. Various nonsurgical and surgical methods have been used to treat this problem.
Nonsurgical Treatment
The first line of non-surgical treatment is medication to restore blood supply and allow new bone growth. Some of the more common drugs used include lipid-lowering (cholesterol-lowering) agents, vasodilators (to open up the blood vessels), anticoagulants (to prevent blood clotting), and bisphosphonates (to prevent bone loss). The type of medication used depends on the underlying systemic disease causing the bone problem. Nonsteroidal antiinflammatory drugs (NSAIDs) may provide some symptom relief of the osteoarthritis but they do not slow or stop the osteonecrosis.
Patients are advised to stop using tobacco or alcohol. Anyone taking corticosteroids should consult with the prescribing physician to review the need for and the use of these medications because of their possible adverse effects on bone.
Physiotherapy is helpful in all stages of the disease but particularly in stage I and stage II when there are few changes seen on X-ray.
Studies show that the overall results of nonsurgical treatment in the shoulder are satisfactory when the disease is caught during the early stages.
Nonsurgical Rehabilitation
What should I expect during treatment?
Physiotherapy at In Step Physical Therapy can be very useful for patients suffering from osteonecrosis of the shoulder, particularly if treatment is begun in the early stages of the disease.
The first goal of our treatment at In Step Physical Therapy is to reduce pain and any inflammation around the shoulder. The use of ice, heat, ultrasound, and other electrical modalities can be very useful as you begin your therapy. Your therapist may also use massage around the shoulder, neck or into the arm, which can help to ease pain and encourage blood flow to the affected area. Gentle mobilizations of the shoulder joint can also be helpful to ease any muscle spasm or pain.
While your therapist is trying to reduce the pain in your shoulder and encourage early healing, they may ask you to avoid lifting your arm overhead or away from your body against resistance. They will also encourage you to avoid lifting or holding anything heavy. They may even give you a weight restriction (i.e., don't lift anything more than two to five pounds or 1-2 kilograms). This restriction will include avoiding some everyday functional activities, such as putting away heavy groceries.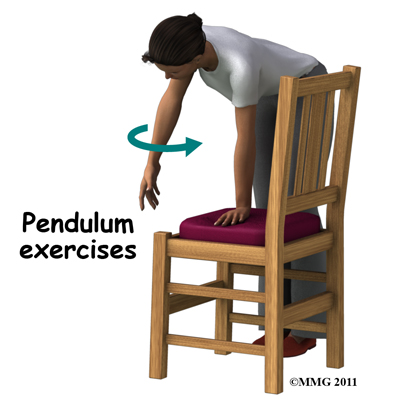 As soon as possible your therapist will begin to work on regaining your shoulder’s motion. They will teach you exercises that you can do yourself to assist with range of motion, which may include the use of sticks or pulleys to help raise the shoulder passively or your therapist may encourage you to partially use the muscles on your affected side (with the assistance of your good side) without causing discomfort. Doing pendular exercises can also help to maintain some shoulder range of motion and assist with pain at this stage. Pendular exercises are performed by leaning forward or to the side, letting the arm hang clear of the chest, and then initiating movement with your trunk so that the dangling limb passively and gently moves. This action provides some traction to the shoulder joint, which aids in pain relief, and also assists the shoulder into a relatively elevated position (in relation to the trunk.) It is important that the pendular activity is done as passively as possible without initiating motion
As soon as possible your therapist will begin to work on regaining your shoulder’s motion. They will teach you exercises that you can do yourself to assist with range of motion, which may include the use of sticks or pulleys to help raise the shoulder passively or your therapist may encourage you to partially use the muscles on your affected side (with the assistance of your good side) without causing discomfort. Doing pendular exercises can also help to maintain some shoulder range of motion and assist with pain at this stage. Pendular exercises are performed by leaning forward or to the side, letting the arm hang clear of the chest, and then initiating movement with your trunk so that the dangling limb passively and gently moves. This action provides some traction to the shoulder joint, which aids in pain relief, and also assists the shoulder into a relatively elevated position (in relation to the trunk.) It is important that the pendular activity is done as passively as possible without initiating motion
from the shoulder muscles. The exercise should look similar to a weighted pendulum that randomly swings gently on the end of a piece of string.
Maintaining your neck range of motion is also very important when your shoulder is not moving well, so your therapist will also prescribe exercises to ensure you can move your neck well for all your daily activities, and that you don’t end up with a stiff neck along with your painful shoulder.
Your therapist may also manually assist your range of motion by stretching or mobilizing your shoulder. Your therapist may need to work on any part of the shoulder joint including the glenohumeral joint, the joint between the shoulder blade and the thorax (scapulothoracic joint), or even the joints where your collarbone joins the trunk and the shoulder (sternoclavicular and acromioclavicular joints.) Your physiotherapist will passively move these joints into their available ranges of motion while you try to relax the muscles of your shoulder completely.
Next, once your pain is under control and your shoulder range of movement is improving, your therapist will focus on strengthening exercises. Your therapist will start by prescribing simple strengthening exercises that only involve isometric strengthening. Isometric strengthening exercises are done by tightening your muscles without actually moving the associated joint. Isometric exercises work the muscles without straining the injured or painful shoulder. Your physiotherapist will teach you how to use your other hand or a wall for resistance while you flex and tighten your muscles, creating an isometric contraction of the shoulder muscles. Your therapist will then progress your exercises so that you are strengthening the muscles through their available ranges of movement, as you are able. More advanced exercises will involve the use of light weights or exercise band to add resistance for your upper limb.
As a result of any injury, the receptors in your joints and ligaments that assist with proprioception (your joint’s sense of position) decline in function. A period of decreased mobility will add to this decline. Proprioception is particularly important when any joint is bearing weight. Although your arm and shoulder girdle are not traditionally thought of as weight-bearing parts of the body, even an activity such as assisting yourself with your arms to get out of a chair or pulling a glass from a cupboard requires weight to be put through or lifted by your shoulder girdle and for your body to be proprioceptively aware of your limb.
Proprioceptive exercises might include activities such as rolling a ball on a surface with your hand, lying on your back while holding and moving a weight up overhead, or pushups on an unstable surface. Advanced exercises may include activities such as ball throwing or catching overhead once you have regained that range of motion.
The proprioceptive control of the shoulder blade (scapula) on the rib cage (scapulothoracic motion) is especially important in being able to use your shoulder girdle and upper limb effectively without causing further injury. Normal scapulothoracic motion is particularly essential once you are able to use your limb near or above shoulder height. For this reason, your physiotherapist will teach you how to properly control your scapula during your rehabilitation exercises as well as during your everyday activities
Your physiotherapist will also remind you about maintaining good shoulder posture even when sitting or using your upper limb during activities that are below shoulder height, such as working on the computer. Rounded shoulders in this position crowds the shoulder joint and can lead to shoulder impingement and pain. It should be noted that regaining proprioception of the shoulder girdle and upper limb requires concentrated work; most people have not previously needed to focus so intently on such controlled motion. The concentrated effort of these shoulder exercises, however, has a substantial reward as it plays a significant part in avoiding associated shoulder problems in the future once the original osteonecrosis problem has been dealt with.
It should be noted that physiotherapy might be needed for extended periods of time. There are some patients whose osteonecrosis will continue to progress despite early conservative care. Unfortunately predicting who might develop a more advanced disease is difficult, so close monitoring is advised. If conservative care fails or the breakdown is too advanced to trial conservative care, surgery may be required.
In Step Physical Therapy provides services for physiotherapy in Edmonton.
Surgery
Core Decompression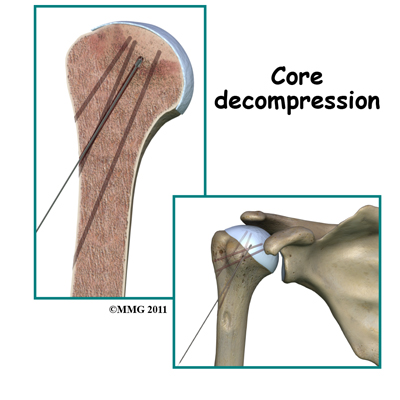 Surgical intervention may be needed in the more advanced stages of osteonecrosis. When the condition is in the early stages, a procedure called core decompression is used to reduce bone marrow pressure and allow the formation of a new blood supply to the area. The new blood vessels help the necrotic area start to form new, healthy bone.
Surgical intervention may be needed in the more advanced stages of osteonecrosis. When the condition is in the early stages, a procedure called core decompression is used to reduce bone marrow pressure and allow the formation of a new blood supply to the area. The new blood vessels help the necrotic area start to form new, healthy bone.
Core decompression is done by drilling small holes from the healthy bone to the area of necrosis in the humeral head. This creates channels that allow new blood vessels to grow into the necrotic area. The surgeon uses a special type of X-ray called fluoroscopy to guide the placement of the pins used to drill the holes. Removing some of the dead bone also causes bleeding into the region of necrotic bone and stimulates new bone growth. Many patients report immediate pain relief from this procedure.
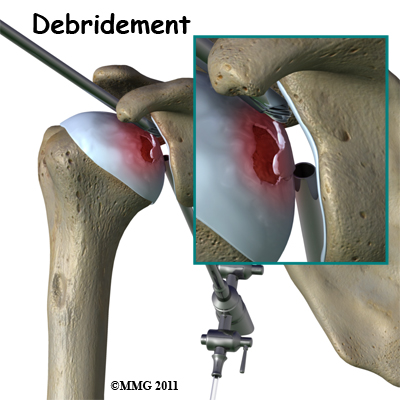
Arthroscopy
If there are any loose bits of bone or cartilage in the joint, then the surgeon may have to perform arthroscopic debridement . The arthroscope is a small fiberoptic camera that can be inserted into the joint allowing the surgeon to see the inside of the joint. Other instruments can be inserted into the joint through small incisions to remove tissue and smooth the surface of the joint. The shoulder joint is cleaned up of any debris. Any frayed edges of joint cartilage are smoothed down. Sometimes the surgeon combines these two procedures (decompression and arthroscopy). The arthroscopic exam shows the location and extent of the disease in the joint while the decompression addresses the necrotic area of bone.
Bone Grafting
Bone grafting replaces the necrotic (dead) bone with donor bone that is usually taken from the patient's own hip. This treatment approach is used for mild to moderate disease. It is not advised for late stage disease as studies show patients with more advanced disease do better with arthroplasty (joint replacement). The bone graft gives the joint surface support needed to keep it from collapsing, and with that support in place, the bone can begin to heal.
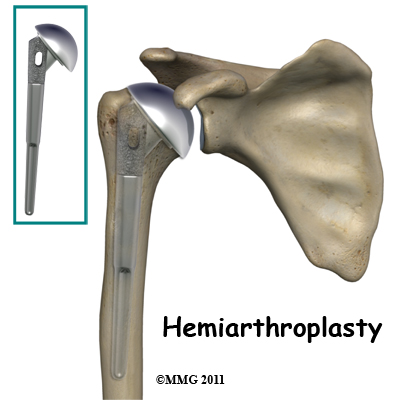
Arthroplasty
Joint replacement is used for more severe damage of the joint. A hemiarthroplasty (partial replacement) may be all that's needed when only one side of the joint has been affected. Full joint replacement is reserved for patients with significant involvement of both the humeral head and the glenoid fossa (socket).
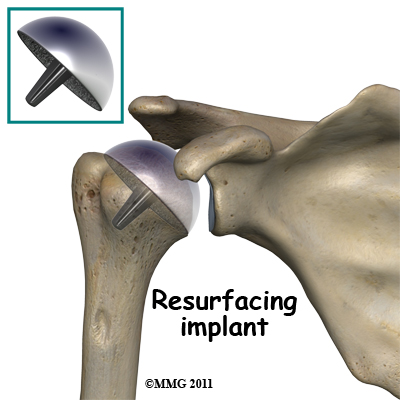
A newer procedure called humeral head resurfacing is gaining popularity and may help save the joint. Instead of removing the head of the humerus and replacing it, the bone is smoothed down and a metal cap placed over the smoothed head like a tooth capped by the dentist. The cap is held in place with a small peg that fits down into the bone. Joint resurfacing requires that the patient have enough healthy bone to support the cap.
Post-surgical Rehabilitation
What should I expect after treatment?
Depending on what you have had done during surgery will determine the appropriate time to begin post-surgical rehabilitation at In Step Physical Therapy. The goal of all therapy after surgery will be to decrease any residual surgical pain, regain range of motion, regain strength, and improve proprioception.
Despite what you have had done during surgery your therapist may use modalities such as ice, heat, ultrasound or electrical modalities to decrease any post-surgical pain or inflammation. They may also massage around your shoulder, into your neck or down your arm, which can also assist with pain and inflammation.
After core decompression surgery, you may be wearing a sling for a few days. Rehabilitation can progress relatively quickly with active-assisted motion being allowed nearly immediately in all directions. Active-assisted exercises are done by using your other hand or holding a stick or pulley to help guide the involved side through the motion and to take part of the weight of the surgical arm. Movements should not be forced and you should only go as far as you can comfortably. Your therapist may mobilize your joint to help regain the needed movements of the shoulder. Strength exercises can begin early on as well and will start with either isometric exercises (see explanation under non-surgical rehabilitation) or by just lifting the weight of your arm. As able, you will progress to using small weights or exercise band for resistance.
After core decompression you will gradually resume all normal activities over a period of four or five weeks, as long as you remain pain free. More stressful activities that load the joint are not allowed for a full year following decompression. Your therapist will be able to advise you over your recovery time when it is appropriate to start doing more stressful activities.
With any of the more invasive procedures, such as joint replacement, major muscles are cut and reattached during the operation therefore regaining motion is progressed more slowly to protect the healing soft tissues. Passive range-of-motion where you do not lift the weight of the arm with the arm’s own muscles, but rather move it through the available range of motion using a pulley or with the other arm can be done early on. Your therapist may also gently mobilize your shoulder joint to assist in gaining range of motion, however aggressive stretching is not allowed until around 12 weeks post-op.
As the shoulder begins to heal, you will be able to start to use the muscles to lift the arm. Generally your therapist will progress you from passive motion through to active-assisted motion and then to full active movement where you are taking the full weight of the arm with its own muscles over a period of approximately six weeks.
Strengthening exercises after one of the more invasive surgical procedures used for humeral head osteonecrosis won’t begin until around 12 weeks post-operatively. At that time your physiotherapist at In Step Physical Therapy will progress you from isometric exercises to light strengthening exercises where you are using weights or exercise band to provide resistance. As tolerated your physiotherapist will progress you to heavier weights and add endurance type exercises.
No matter which surgical procedure you have undergone, your physiotherapist will prescribe proprioception type exercises as your shoulder tolerates it. As explained in detail under non-surgical rehabilitation, proprioception exercises assist your body in knowing where your joints and limbs are in space, and are crucial to returning your surgical joint back to its functional use.
Results of surgical treatment are often good but patients should be prepared for the possibility that osteonecrosis of the humeral head can progress over time and that further surgery may be needed. Sometimes for those patients who have had decompression or bone grafting, joint replacement may eventually be needed. For these reasons, if your therapy is not progressing as your therapist would expect, they will ask you to follow up with your surgeon to ensure that there are no hardware issues inside the joint or other problems within the shoulder that are impeding your progress.
Portions of this document copyright MMG, LLC
In Step Physical Therapy provides services for physiotherapy in Edmonton.




