Lumbar Artificial Disc Replacement
|
||||||
Introduction
Physiotherapy in Edmonton for Lower Back
Welcome to In Step Physical Therapy's patient resource about Lumbar Artificial Disc Replacement.
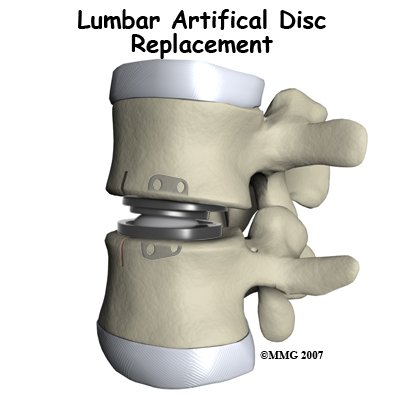
Artificial disc replacement (ADR) is a device or implant used to replace a diseased or damaged intervertebral disc.After removing what’s left of the worn out disc, the ADR is inserted in the space between two lumbar vertebrae. The goal is to replace the diseased or damaged disc while keeping your normal spinal motion. Artificial disc surgery is relatively new in the United States but has been used in Europe for many years. In the U.S., the first lumbar artificial disc surgery was done in clinical trials in October 2001. The Federal Drug Administration (FDA) approved the use of the lumbar ADRs in October 2004.
This guide will help you understand:
- what parts of the spine are involved
- what your surgeon hopes to achieve
- who can benefit from this procedure
- what happens during the procedure
- what to expect as you recover
#testimonialslist|kind:all|display:slider|orderby:type|filter_utags_names:Back Pain|limit:15|heading:Hear from some of our patients who we treated for *Back Pain*#
Anatomy
What parts of the spine are involved?
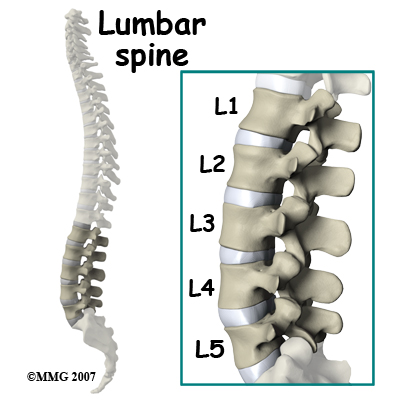
The human spine is made up of 24 spinal bones called vertebrae. Vertebrae are stacked on top of one another to form the spinal column. The spinal column gives the body its form. It is the body's main upright support. The section of the spine in the lower back is known as the lumbar spine. Lumbar disc replacement typically occurs in the lumbar spine (from L4-S1).
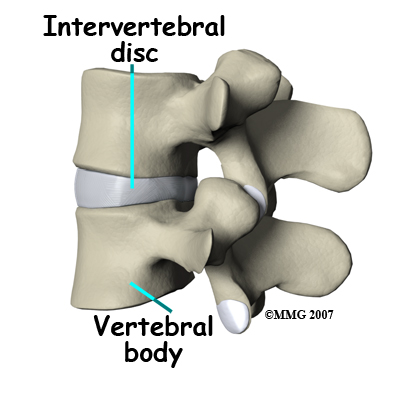
An intervertebral disc sits between each pair of vertebrae. The disc normally works like a shock absorber. It protects the spine against the daily pull of gravity. It also protects the spine during strenuous activities that put strong force on the spine, such as jumping, running, and lifting.
An intervertebral disc is made of two parts. The center, called the nucleus is spongy. It provides most of the disc's ability to absorb shock. The nucleus is held in place by the annulus, a series of strong ligament rings surrounding it. Ligaments are connective tissues that attach bones to other bones.
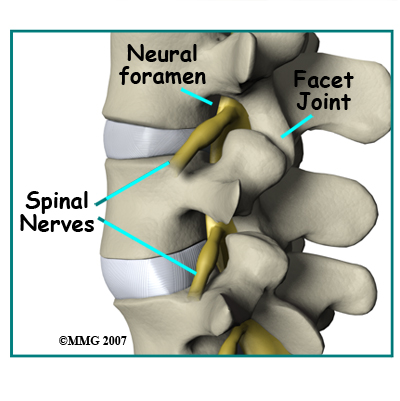
Between the vertebrae of each spinal segment are two facet joints. The facet joints are located on the back of the spinal column. There are two facet joints between each pair of vertebrae, one on each side of the spine. A facet joint is made of small, bony knobs that line up along the back of the spine. Where these knobs meet, they form a joint that connects the two vertebrae. The alignment of the facet joints of the lumbar spine allows freedom of movement as you bend forward and back.
From the side, the spine forms three curves. The neck, called the cervical spine, curves slightly inward. The middle back, or thoracic spine, curves outward. The outward curve of the thoracic spine is called kyphosis. The low back, also called the lumbar spine, curves slightly inward. An inward curve of the spine is called lordosis.
Related Document: In Step Physical Therapy's Guide to Lumbar Spine Anatomy
Rationale
What does the surgeon hope to achieve?
Disc replacement surgery is done to stop the symptoms of degenerative disc disease. Discs wear out or degenerate as a natural part of aging and from stress and strain on the spine. Eventually, the problem disc collapses, which causes the vertebra above to sink toward the one below. This loss of disc height affects nearby structures – especially the facet joints.
When the disc collapses it no longer supports its share of the load in the spine. The
facet joints of the spine begin to support more of the force that is transmitted between each vertebra. This increases the wear and tear on the articular cartilage that covers the surface of the joints. The articular cartilage is the smooth, slippery surface that covers the surface of the bone in any joint in the body. Articular cartilage is tough, but it does not tolerate abnormal pressure well for long. When damaged, articular cartilage does not have the ability to heal. This wear and tear is what is commonly referred to as arthritis.
Shrinking disc height also reduces the size of the neural foramina, the openings between each vertebral pair where the nerve roots leave the spinal column. The arthritis also results in the development of bone spurs that may protrude into these openings further narrowing the space that the nerves have to exit the spinal canal. The nerve roots can end up getting squeezed where they pass through the neural foramina.
Replacing the damaged disc with an artificial disc, or implant, called a prosthesis can restore the normal distance between the two vertebrae. The artificial disc sits between the two vertebrae and distracts or jacks up the upper vertebra. Enlarging the disc space relieves pressure on the facet joints. It also opens up the space around the spinal nerve roots where they pass through the neural foramina.
Another benefit of the artificial disc replacement is that it mimics a healthy disc. Natural motion is preserved in the spine where the new disc is implanted. And it helps maintain stability in the spinal joints above and below it.
Who can benefit from this procedure?
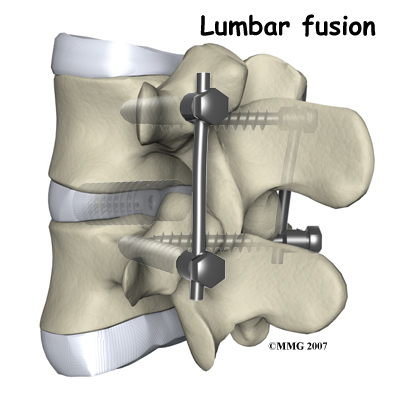
For many years, the standard of care for chronic pain from a degenerated disc has been spinal fusion surgery. Bone graft donated by a bone bank or taken from your pelvic bone is used to fuse two or more vertebral bones together.The spine is stabilized but you will lose motion at that level. The increased stress on the next lumbar vertebra can cause problems later.
The artificial disc replacement is used to reduce or eliminate the pain while still allowing motion. One advantage of the artificial disc is that it may also prevent premature breakdown of adjacent levels of the lumbar spine.
You may be a good candidate for a lumbar artificial disc replacement if you have chronic pain and disability from lumbar disc degeneration despite nonoperative treatment for at least six months. The artificial disc replacement provides an alternative to spinal fusion. The device helps restore the normal space between two vertebrae. You will still have movement at the level where the ADR is implanted.
Preparation
How should I prepare for surgery?
Knowing what to expect before and after surgery can help you plan for recovery at home. Once you and your surgeon have agreed that disc replacement surgery is indicated, certain preparations for the surgery are important.
You may need to visit your primary care physician or internal medicine specialist to obtain medical clearance for surgery. This will ensure that you are in the best medical condition prior to the surgery. A doctor who will be performing your anesthesia (an anesthesiologist) will evaluate and counsel you regarding anesthesia.
Certain factors put you at increased risk for problems during or after the operation. It’s best to reduce or eliminate as many of these risk factors as possible. For example, the use of alcohol or other drugs (including tobacco) can be major factors in how your body copes with anesthesia and the stress of surgery.
You should stop any anti-inflammatory medications 10 days before surgery. If you aren’t sure which medications this includes, ask your doctor. You should stop smoking or using tobacco as soon as possible but at least two weeks before surgery. This is very important to reduce complications from heart and lung problems. Smoking also decreases the success rate of spine surgery. Stopping smoking will increase your chance of a successful result.
You may need to donate one or two units of your own blood. This blood will be stored in the blood bank until surgery. If you need a transfusion either during or after your surgery you will receive your own blood back.
On the day of your surgery, you will probably be admitted to the hospital early in the morning. You shouldn't eat or drink anything after midnight the night before. Let your surgeon know if you have diabetes and how you manage it (insulin pump, insulin injections, diet, exercise). Your need for insulin can change as a result of the stress of hospitalization and surgery. Even if you are tightly controlled now, you should monitor your glucose levels closely for at least a week before surgery and continue to do so for several weeks after surgery.
Surgical Procedure
What happens during the operation?
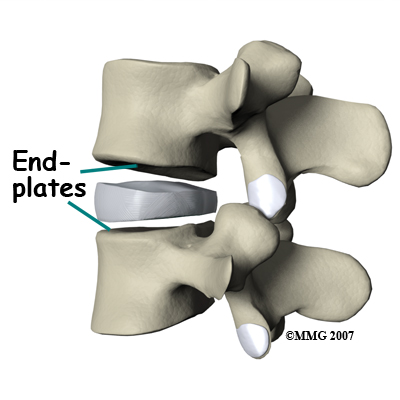
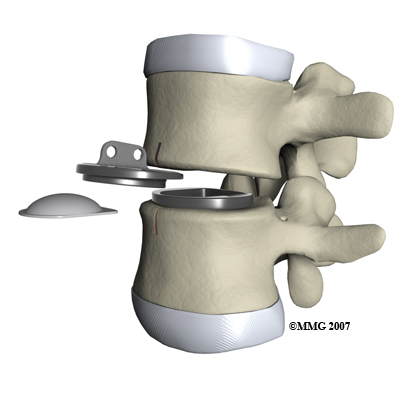
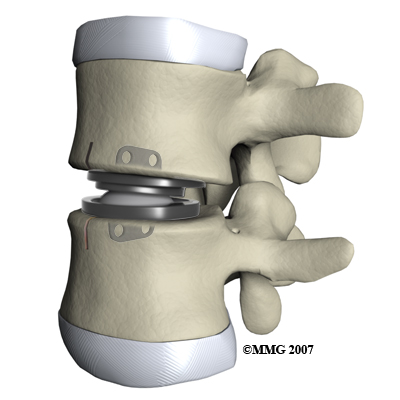
Before we describe the procedure, let’s look first at the artificial disc itself. The lumbar artificial disc has several different designs. They are made of metal, ceramic, and plastic. Some look like a sandwich with two endplates separated by a plastic spacer. The two endplates are made of cobalt chromium alloy, a safe material that has been used for many years in replacement joints for the hip and knee.

A plastic (polyethylene) core fits in between the two metal endplates. The core acts as a spacer and is shaped so that the endplates pivot in a way that imitates normal motion of the two vertebrae. There are small prongs or teeth on one side of each endplate. The teeth help anchor the endplate to the surface of the vertebral body.
Another way of anchoring the artificial disc replacement is the central keel or fin design. The implant is secured to the vertebral end plates by a thin, upright piece of metal that looks like the rudder on a boat or a shark’s fin.
Another artificial disc replacement design is a ball and socket articulation to allow for normal translation of motion at that segment. The implant may be made of titanium and polyurethane in a metal-on-plastic design. Some are made of stainless steel and are all metal-on-metal.
Inserted between two vertebrae, the prosthesis reestablishes the height between two vertebrae. As a result of enlarging the disc space, the nearby spinal ligaments are pulled tight, which helps hold the prosthesis in place. The prosthesis is further held in place by the normal pressure through the spine.
The lumbar artificial disc replacement comes in a variety of sizes and angles. There are constrained and unconstrained designs. The constrained devices provide a fixed center of rotation that doesn’t change. The unconstrained design allows the center of the implant to move forward and back slightly during lumbar motion. The surgeon can also choose an implant with the correct angle for each patient in order to build in the right amount of lordosis (spinal curvature).
The Operation
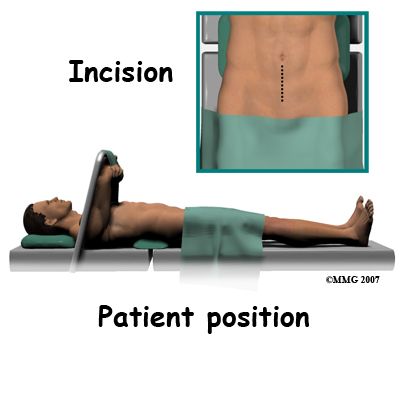
Lumbar ADR is done through the anterior ( front) of the spine. For your safety there are usually two surgeons present; your spine surgeon and a general or vascular surgeon.
The new system is placed in the spine through an incision though the abdomen or belly. Working from the front of the spine through the abdomen, the organs are carefully moved to one side. This makes it easier to see the front of the spine. The spine surgeon removes a large section from the middle of the damaged disc.
Next, the bones of the spine are spread apart to make more room to see and work inside the disc space. Using a surgical microscope, any remaining disc material toward the back of the disc is removed. The surgeon will also remove any disc fragments pressing against the nerve and shave off any osteophytes (bone spurs).
The disc space is distracted (jacked up) to its normal disc height. This step helps decompressor take pressure off the nerves. At this point, x-rays or a fluoroscope, is used to insert the artificial disc device into the prepared disc space. The fluoroscope is an x-ray machine that allows the surgeon to actually see an x-ray image while doing the procedure. Using a fluoroscope, the surgeon is able to see where the implant goes as it is inserted. This makes the procedure much safer and much more accurate.
Finally, moving the spine in various positions tests the prosthesis. An X-ray may be taken to double check the location and fit of the new disc.
Complications
What might go wrong?
All types of spine surgery, including artificial disc replacement, have certain risks and benefits. Complications from any kind of surgery can also occur from anesthesia, infection, and development of blood clots (thrombophlebitis). Medical complications arising from spinal surgery are rare but could include stroke, heart attack, spinal cord or spinal nerve injury, pneumonia, or possibly death.
Your spine surgeon will discuss the most common complications with you. This document will help you prepare any questions you may have. It doesn’t provide a complete list of all the possible complications. Complications from the artificial disc replacement procedure are rare and are lower than for spinal fusion. Results continue to improve with advances in technology and better surgical techniques. The more common problems may include but are not limited to:
- problems with anesthesia
- thrombophlebitis (blood clots)
- infection
- nerve damage or paralysis
- spontaneous ankylosis (fusion)
- problems with the implant
- retrograde ejaculation (men only)
- ongoing pain
Anesthesia Complications
Problems can arise when the anesthesia given during surgery causes a reaction with other drugs you may be taking. In rare cases, a patient may have problems with the anesthesia itself. In addition, anesthesia can affect lung function because the lungs don't expand as well while a person is under anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
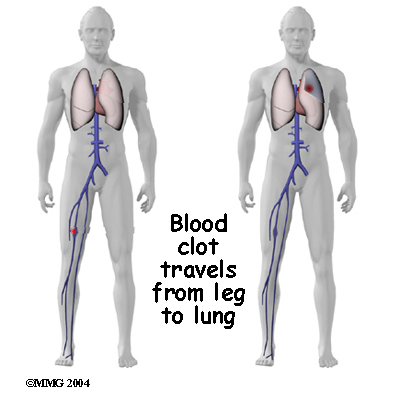 Thrombophlebitis (Blood Clots)
Thrombophlebitis (Blood Clots)
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can happen after any operation. It occurs when blood in the large veins of the leg forms blood clots. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible after surgery. Two other commonly used preventative measures include
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Infection
Infection following spine surgery is rare but can be a very serious complication. Some infections may show up early, even before you leave the hospital. Infections on the skin's surface usually go away with antibiotics. Deeper infections that spread into the bones and soft tissues of the spine are harder to treat. They may require additional surgery to treat the infected portion of the spine.
Nerve Damage or Paralysis
Any surgery that is done near the spinal canal can potentially cause injury to the spinal cord or spinal nerves. Injury can occur from bumping, stretching, or cutting the nerve tissue with a surgical instrument. Nerve involvement can cause nerve pain, muscle weakness, and a loss of sensation to the areas supplied by the nerve.
These symptoms are usually temporary and will gradually go away in one to three months’ time. Swelling around the nerve or the formation of scar tissue can also result in pressure or traction on the nerve. Scar tissue called fibrosis does not always resolve resulting in chronic pain and long-term weakness and sensory changes.
Spontaneous Ankylosis
Scientists aren’t sure why but sometimes the spine fuses itself, a process called spontaneous ankylosis. Loss of spinal motion is the main side effect of this problem. Bone may also form in the soft tissues around the vertebrae. For example, cartilage turns to bone or bone-like tissue. This process is called ossification. Ossification may or may not affect the implant or your final results in terms of motion or function.
Problems with the Implant
The prosthesis itself can sometimes be a source of complications. Although rare, the prosthesis can shift out of its normal position and even dislocate. If the implant migrates out of position, it can cause injury to the nearby tissues. A second surgery may be needed to align or replace the implant.
And similar to other types of joint replacements, the artificial disc may fail over time if the parts wear out. Your ADR is estimated to last 15 to 20 years. If the disc moves out of position or wears out, it can be removed. When surgery is done to take out the original prosthesis, a fusion surgery will most likely be recommended.
Subsidence is another possible problem. The implant actually sinks down into the vertebral body above or below it. This results in a loss of the normal disc height. Neurologic compression with neurologic symptoms can occur.
Over time, wear and tear just from the physical process of motion across a bearing surface can cause tiny bits of debris to flake off the implant. The body may react to these particles with an inflammatory response that can cause pain, implant loosening, and implant failure. So far, significant inflammatory reactions have not been reported for spinal ADRs.
Retrograde Ejaculation
Lumbar disc replacement surgery carries risks associated with operating from the front of the spine. In men, the anterior approach can also sometimes result in a complication called retrograde ejaculation.
Tiny nerves in front of the lower spine may be damaged during the anterior approach. If so, semen enters the bladder instead of going out through the urethra during ejaculation. Male patients planning a family might wish to consider donating sperm before surgery. Studies have not reported cases of sexual dysfunction but it is a potential risk.
Ongoing Pain
Not all patients get complete pain relief with this procedure. As with any surgery, patients should expect some pain afterward. If the pain continues or becomes unbearable, talk to your surgeon about treatments that can help control your pain.
After Surgery
What happens after surgery?
You may have immediate relief from your painful symptoms, but many people notice a gradual improvement over the next weeks to months. Many patients are able to reduce or eliminate the use of pain medication as well.
Your hospital stay will depend on how quickly you recover but most people are able to go home by the third day after surgery. You may require an extra day or two if for some reason you’re having extra pain or unexpected difficulty.
Most people recover quickly after the artificial disc procedure. You will be getting up out of bed and walking the same day as your surgery. You may even be able to get out of bed and walk within a few hours. Move carefully and comfortably, and avoid extending your back (bending backward). You probably won’t need a back brace or other support while the tissues are healing.
When you go home, you should be safe to sit, walk, drive, and ride a bike. Lifting anything more than eight to 10 pounds should be avoided for at least four weeks. To help you gauge what you can and can’t lift, keep in mind that a gallon of milk weighs about eight pounds.
Your surgeon will continue to follow-up with you. X-rays will be done from time to time to make sure the implant is still in its proper place. Your surgeon will let you know when you can return to work. Depending on the type of work you do, this should be in about two to four weeks. If your job requires moving and lifting heavy items, you may need a longer period of recovery. Your surgeon may give you the okay to do all your activities by the sixth week after surgery. You can expect to return to previous recreational activity by the end of three months.
Portions of this document copyright MMG, LLC.
Our Rehabilitation
What should I expect as I recover?
After you leave the hospital, your physiotherapist at In Step Physical Therapy can develop a personalized home program of exercises and activities to help you regain motion and function. It’s important to continue with your walking program on a daily basis when you go home. Your goal should be to walk at least 30 minutes at a moderately brisk pace at least five days each week.
Although the time required for recovery is different for each patient, as a general rule, our patients recovering from Lumbar Artificial Disc Replacement attend physiotherapy two to three times each week for about four to six weeks.
Our physiotherapist will recommend active treatments to improve flexibility, strength, and endurance. Gentle stretching exercises for the back are commonly prescribed. We will have you begin a series of strengthening exercises to help tone and control the muscles that stabilize the trunk and back. It is also important to build strength in your legs. The endurance exercises that we recommend may include treadmill walking, swimming, or stationary biking.
When your symptoms are under control and you’re comfortable doing your exercises, your formal therapy sessions at In Step Physical Therapy will end. Although we will continue to be a resource, you will be in charge of doing your exercises as part of an ongoing home program.
In Step Physical Therapy provides services for physiotherapy in Edmonton.
Summary
Artificial disc replacement may offer an alternative to spinal fusion for some patients who have chronic back pain from degenerative disc disease. While fusion stops pain by eliminating movement in the problem spinal segment, artificial disc replacement allows natural motion in the part of the spine where the disc is implanted. This is because the prosthesis is designed to restore normal motion and height between adjacent vertebrae. Artificial disc replacement allows for an early return to function.
The implant is designed to withstand bending, twisting, compression and repeated loads during movement. For active adults, successful disc replacement should endure years of high loads without mechanical failure.
Long-term studies to assess the safety and effectiveness of artificial disc replacements are ongoing. Researchers are looking at the impact of the ADR on other discs and on the bony structures of the spine. So far results show a low rate of complications. There have been no reports of death, significant infection, or major neurological problems. Patient satisfaction is good to excellent in most, but not all, cases.
Portions of this document copyright MMG, LLC.




