Bipartite Patella
|
||||||
Physiotherapy in Edmonton for Knee Issues
Welcome to In Step Physical Therapy's resource about Bipartite patella.
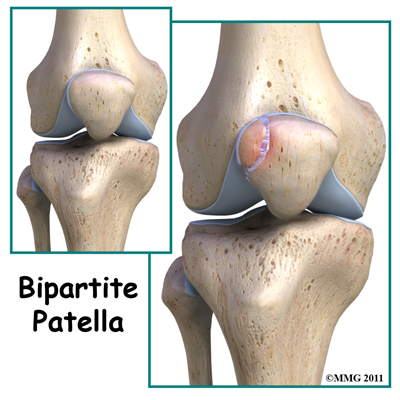 Bipartite patella is a congenital condition (present at birth) that occurs when the patella (kneecap) is made of two bones instead of a single bone. Normally, the two bones would fuse together as the child grows but in bipartite patella, they remain as two separate bones. About one per cent of the population has this condition. Boys are affected much more often than girls. When this condition is discovered in adulthood it is often an “incidental finding” meaning that when your health care professional was investigating another problem around the knee, the bipartite patella is discovered.
Bipartite patella is a congenital condition (present at birth) that occurs when the patella (kneecap) is made of two bones instead of a single bone. Normally, the two bones would fuse together as the child grows but in bipartite patella, they remain as two separate bones. About one per cent of the population has this condition. Boys are affected much more often than girls. When this condition is discovered in adulthood it is often an “incidental finding” meaning that when your health care professional was investigating another problem around the knee, the bipartite patella is discovered.
This guide will help you understand:
- what parts of the knee are involved
- how this condition develops
- how health care professionals diagnose this condition
- what treatment options are available
- what In Step Physical Therapy’s approach to rehabilitation is
#testimonialslist|kind:all|display:slider|orderby:type|filter_utags_names:Knee Pain|limit:15|heading:Hear from some of our patients who we treated for *Knee Pain*#
Anatomy
What is the patella and what does it do?
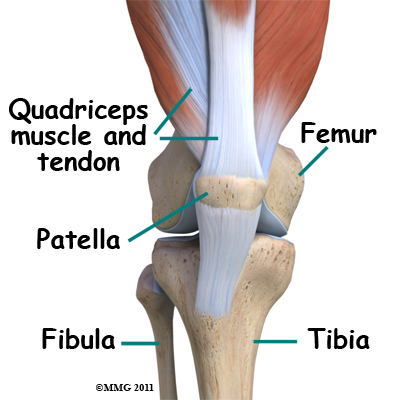
The knee is the meeting place of two important bones in the leg, the femur (the thighbone) and the tibia (the shinbone). The patella (kneecap) is the moveable bone that sits in front of the knee. This unique bone is wrapped inside a tendon that connects the large muscles on the front of the thigh, the quadriceps muscles, to the lower leg bone.
Related Document: In Step Physical Therapy's Guide to Knee Anatomy.
Causes
What causes this condition?
In development the patella starts out as a piece of fibrous cartilage. It only turns into bone or ossifies as part of the growth process. Each bone has an ossification center. This is the first area of the structure to start changing into bone.
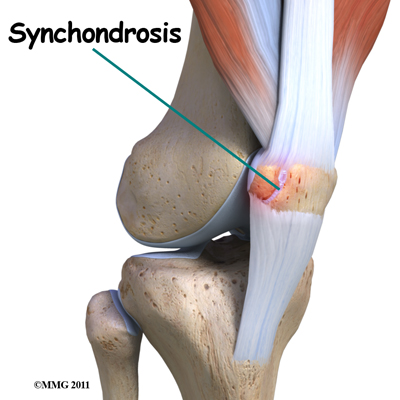
Most bones (including the patella) only have one primary ossification center. In some cases, however, a second ossification center is present. Normally, these two centers of bone will fuse together during late childhood or early adolescence. If the bones do not ossify together, then the two pieces of bone remain connected by fibrous or cartilage tissue. This connective tissue is called a synchondrosis.
 In the patella the most common location of the second bone is the supero-lateral (upper outer) corner of the patella but the bone can be at the bottom of the patella or along the side of the kneecap.
In the patella the most common location of the second bone is the supero-lateral (upper outer) corner of the patella but the bone can be at the bottom of the patella or along the side of the kneecap.
Injury or direct trauma to the synchondrosis can cause a separation of this weak union between the two bones, which then leads to inflammation. Repetitive micro trauma can have the same effect. The cartilage has a limited ability to repair itself. The increased mobility between the main bone and the second ossification center further weakens the synchondrosis resulting in painful symptoms.
Symptoms
What does bipartite patella feel like?
Most of the time, there are no symptoms. Sometimes there is a bony bump or place where the bone sticks out more on one side than the other. If inflammation of the fibrous tissue between the two bones occurs, then painful symptoms develop directly over the kneecap. The pain is usually described as a dull ache. There may be some swelling.
Movement of the knee can be painful, especially when bending the joint. Atrophy of the quadriceps and misalignment of the patella can lead to patellar tracking problems. Squatting, stair climbing, weight training, and strenuous activity will all aggravate the knee causing increased symptoms. For the runner, running down hill in particular causes increased pain, tenderness, and swelling.
Diagnosis
How will my health care professional diagnose this condition?
Most of the time, this condition is seen on X-rays of the knee that are taken for some other reason. This is referred to as an incidental finding. Sometimes, it is mistaken for a fracture of the patella but since the problem usually affects both knees, an X-ray of the other knee showing the same condition can confirm the diagnosis.
If, due to the proper mechanism of injury being present, a fracture is suspected, then MRIs or bone scans are useful if the fracture doesn’t show up on the X-rays. The presence of fibrocartilaginous material between the two bones on MRI helps confirm a diagnosis of bipartite patella. An MRI can also show the condition of articular cartilage at the patellar-fragment interface. The lack of bone marrow edema helps rule out a bone fracture. CT scans will show the bipartite fragment but are not as helpful as MRIs because bone marrow or soft tissue edema does not show up, so it’s still not clear from CT findings whether the symptoms are from a fragment or a fracture.
Treatment
What treatment options are available?
Most of the time, no treatment is necessary because most people who have a bipartitepatella, probably don’t even know it. However if an injury occurs and/or painful symptoms develop, then treatment may be needed.
Nonsurgical Treatment
Conservative care involves rest, over-the-counter nonsteroidal antiinflammatory drugs (NSAIDs) such as ibuprofen, and rehabilitation at In Step Physical Therapy.
If there has been a separation of the synchondrosis this can be treated with immobilization for four to six weeks. The knee is placed in full extension using a cast, knee immobilizer, or dynamic patellar brace.

An immobilizer is a removable splint. It’s usually only taken off to wash the leg and remains in place the rest of the time. The dynamic brace immobilizes the knee in an extended (straight-leg) position with limited flexion (up to 30 degrees). The brace reduces pain by decreasing the pull on the patella from the quadriceps muscle. Once healing occurs and the cast or brace is no longer needed, then rehabilitation at In Step Physical Therapy should begin. Once the X-ray shows complete ossification of the two bone fragments, then you should be able to return to your regular activities providing you have also met your rehabilitation goals.
Rehabilitation
What should I expect during treatment?
Nonsurgical Rehabilitation
If you have developed symptoms from bipartite patella then rehabilitation at In Step Physical Therapy can be very useful. If you have been immobilized then your rehabilitation can begin once your immobilizer has been removed.
During your first visit to In Step Physical Therapy your physiotherapist will begin by educating you on activity modification and implementing a period of active rest so that your symptoms calm down. Taking an active rest means decreasing your activity intensity or duration such that you are not aggravating your knee. It means that you can do some activity as long as it does not stir up your knee symptoms. Some activities, however, may need to be completely avoided or replaced by less stressful ones. In most cases avoiding movements such as deep flexion of the knee during activities such as squatting will be advised. Avoiding excessive use of the stairs, as well as resisted weight training will also advised. Often activities such as cycling (with the bike seat high to avoid excessive knee flexion) or cardiovascular activities in the pool can be continued as long as they do not bring on symptoms. If symptoms continue even once you have modified your activity then a complete rest from the activity is the next step.
Your physiotherapist may use electrical modalities such as ultrasound or interferential current to help ease your pain or decrease any swelling that may exist. Ice or heat over the knee can also help with these symptoms. Your therapist can advise you whether ice or heat would be best in your individual case, and you should then also apply this at home.
Your physiotherapist may use tape or a flexible brace to assist with your symptoms. The aim of this treatment is to help guide the kneecap through its proper range of motion while you move the knee during your rehabilitation exercises and during everyday activity. If either the tape or the flexible brace helps your symptoms, your therapist can teach you how to use and apply them yourself on a daily basis. Often a short period where your pain is reduced can allow your symptoms to subside as well as allow a period where strengthening exercises can be most advantageous.
Once your symptoms begin to subside your physiotherapist will start you on some gentle stretching exercises in order to ensure you maintain your full knee range of motion. If you have been immobilized by a brace or cast then your leg may be particularly stiff into bending. Gentle stretches for the quadriceps muscle, which is on the top of the thigh, will be prescribed. There are several modifications of a quadriceps stretch that can be taught if the stretch brings on your symptoms, so be sure to tell your physiotherapist if you are experiencing any pain at all while stretching. In addition to stretching the quadriceps, your therapist may also prescribe other related stretches such as ones for the hip flexors which are at the front of the hip, the hamstrings on the back of the thigh, the buttocks muscles, the calf, or the tensor fascia latae, which is on the upper and outer side of the hip. All of these muscles, if tight, can alter the biomechanics of the knee and put undue stress on the kneecap.
Your physiotherapist will also prescribe strengthening exercises for your knee and lower extremity. It is very important that only the necessary forces are put through your knee in order to avoid future problems with the joint. In order to do this, you need adequate strength in your quadriceps and buttocks muscles, which are the main controllers of the knee position. Your therapist will assess both your lower extremity alignment as well as the strength of the muscles in your lower extremities, which help to maintain your alignment. If there are other muscles, aside from your quadriceps and buttocks muscles that require strengthening, exercises for these muscles will also be prescribed. If strengthening your knee brings on your symptoms and your exercises can not be modified enough to relieve the symptoms then your physiotherapist may suggest that you do strengthening exercises in a hydrotherapy pool rather than on the land. The hydrostatic properties of the water along with the warmth of the water often makes it easier to exercise and to do so with less pain. As soon as possible, though, your exercises should be progressed to land-based exercises as these more closely simulate everyday activities.
As soon as you are able your therapist will progress your strengthening activities so that you incorporate more advanced exercises for your knee. Exercises such as jumping, squatting, stair climbing or descending, or working with heavier lower extremity weights will be added as your physiotherapist feels your knee can tolerate it. Exercise bands, exercise machines, or free weights may be used for additional resistance during the exercise. As stated previously, it is crucial that you do not overload your knee such that you cause any symptoms. Your physiotherapist will be the key to monitoring and advancing your rehabilitation program in order for you to improve as quickly as possible without causing any undue stress on the knee.
The ability to know where your knee is in space without looking at it is called proprioception. Any injury or pain associated with a joint will decrease the joint’s proprioceptive ability. A period of immobilization will add to this decline. Your therapist will prescribe exercises for your proprioception to help your knee function at its peak. Adequate proprioception also assists in avoiding future injuries. Exercises such as balancing on one leg or on an unstable surface such as a wobbly board or a foam disc work your proprioception. Closing your eyes during these exercises challenges your proprioception even further. Advanced proprioceptive exercises may involve hopping, jumping and landing from a height, or moving rapidly from side to side. As with stretching and strengthening exercises, any pain during proprioceptive exercises should be heeded. Eventually exercises that mimic your everyday activities and sporting interests will be added in order to maximally challenge your knee as well as prepare you to return to your regular activity.
It is crucial that proper alignment and technique is maintained throughout all exercises, therefore your physiotherapist will continually draw your attention to your form. The knee is a joint that is particularly sensitive to poor alignment, which causes undue tension on the joint and eventually leads to pain and early wear down of the joint. If necessary, your therapist may suggest the use of foot orthotics or arch taping in order to assist your lower extremity alignment. Lower extremity alignment begins from the ground up, therefore poor foot alignment immediately affects the position and tension on the knee.
In addition to range of motion, strength, and proprioceptive exercises at In Step Physical Therapy, we also highly recommend maintaining the rest of your body’s fitness with regular exercise while you rehabilitate your knee. An upper body bike is a good cardiovascular activity that will not flare up your knee. A stationary bike is also a good cardiovascular activity you can trial, as it generally does not flare up the knee if done with a few simple modifications. Keeping the resistance low on the bike and putting the bike seat up higher than usual help to ensure that you do not experience pain in your knee. If the stationary cycle or other land based activities are too difficult, often a cardiovascular activity in the pool can be performed without irritating your knee. In addition to a cardiovascular activity, weights for your upper extremities and unaffected leg are also strongly encouraged. Advanced exercises such as the stepper or elliptical machines may be used once your knee has recovered to an acceptable level. Running is generally the final activity added to your rehabilitation and cardiovascular program due to the extreme force it exerts through your knee and body in general. Your physiotherapist at In Step Physical Therapy can provide a program for you to maintain your general fitness while you rehabilitate your knee, and can advise you on the best time to advance your cardiovascular exercises without stirring up symptoms.
Most patients with bipartite patella respond well to a period of immobilization and/or rehabilitation along with activity modification. If, however, there is no improvement after three months of conservative care, then surgery is considered.
In Step Physical Therapy provides services for physiotherapy in Edmonton.
Surgery
If conservative care with immobilization is not successful in alleviating swelling and pain, then surgery may be suggested. When the bipartite fragment is small, then the surgeon can simply remove the smaller fragment of bone. When the bipartite fragment is larger and also contains part of the joint surface, the surgeon may decide to try and force the two fragments to heal together or fuse. The connective tissue between the two fragments is removed first and the two bony fragments are then held together or stabilized with a metal screw or pin. This technique is called internal fixation. The two fragments of bone eventually heal together or fuse, creating a solid connection between the two fragments. Although successful in reuniting the patella, the procedure may require several weeks of immobilization. As a result, knee stiffness may occur. Physiotherapy at In Step Physical Therapy is then required once the bones have healed in order to regain motion as well as strength, endurance, and proprioception.
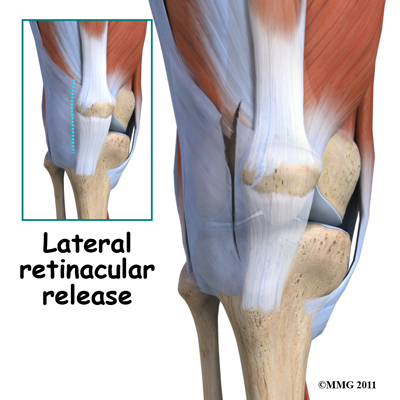
Another potential surgical treatment option is a procedure called a lateral
retinacular release. The vastus lateralis tendon (a part of the large quadriceps muscle
of the thigh) exerts a constant lateral pull on the patella. In patients with bipartite patella this pull is usually on the bone of the bipartite fragment of the upper, outer patella. Simply cutting the vastus lateralis attachment reduces the constant pull on the bony fragment. Healing of the two bony fragments may occur as a result of the decreased tension.
Post Surgical Rehabilitation
Rehabilitation after surgery for bipartite patella should begin as soon as your surgeon indicates that it is safe to do so. What has been done in surgery will determine whether you need a period of immobilization or rest before beginning rehabilitation. Each surgeon will set his or her own specific restrictions regarding when to begin treatment at In Step Physical Therapy based on what was done during the surgical procedure, their personal experience, and whether your tissues are healing as expected.
You may be required to use crutches for a short period after your surgery. If you are still using crutches by the time we first see you at In Step Physical Therapy, your physiotherapist will ensure you are using the crutches safely, properly, and confidently, and that you are abiding by your weight bearing restrictions if you have been given any. We will also ensure that you can safely use your crutches on stairs. If you are no longer using crutches, or once you no longer need them, your physiotherapist will focus on normal gait re-education so you are putting only the necessary forces through your surgical side with each step, and are not compensating in any way. Until you are able to walk without a significant limp, we recommend that you continue to use crutches, or at least one crutch or a cane/walking stick. Improper gait can lead to a host of other pains in the knee, hip and back so it is prudent to use a walking aid until near normal walking can be achieved. Your In Step Physical Therapy physiotherapist will advise you regarding the appropriate time for you to be walking without any walking aid at all.
During your first few appointments at In Step Physical Therapy your physiotherapist will focus on relieving any pain and inflammation that you may be lingering from the surgical procedure itself. We may use modalities such as ice, heat, ultrasound, or electrical current to assist with decreasing any pain or swelling you have around the surgical site or anywhere down the leg. In addition, your physiotherapist may massage your leg and ankle to improve circulation and help decrease pain and swelling.
The next part of our treatment will focus on regaining the range of motion in your knee.
Your physiotherapist at In Step Physical Therapy will prescribe a series of exercises that you will practice in the clinic and also learn to do as part of a home exercise program. Range of motion in the knee generally comes back very quickly after surgery for bipartite patella, but it still depends on exactly what your surgeon has done inside your joint, how much swelling is present, and how controlled your discomfort is. During the range of motion exercises you may experience a small amount of discomfort at the end ranges of motion initially. Despite this discomfort it is still important to perform the range of motion exercises prescribed because moving the joint also helps to move the swelling, get fresh blood to the healing area, and provide nutrition to the surface of the joint.
Only mild discomfort, however, is permissible. Any sharp or moderate discomfort should be heeded. An exercise bike at this stage of your rehabilitation is very useful to assist in gaining back knee range of motion. Even if you are unable to fully rotate the pedals of the bike, using it is still encouraged. Performing the simple back and forth motion forces fluid through the joint, which helps to move the swelling and bring fresh blood to the healing tissues.
In regard to range of motion the goal after surgery for bipartite patella is to regain full bending and extending of your knee joint. Without this full range of motion, areas of the joint surface cartilage can become weak and start to wear down. In addition, without full range of motion the biomechanics of the knee do not function as they have been designed to, and this also contributes to early wearing down of the joint.
In addition to you yourself doing range of motion exercises your physiotherapist may mobilize your knee joint to assist in regaining motion. This hands-on technique encourages the knee to move gradually into its normal range of motion. Mobilization of the knee (including the patella) may be combined with therapist-assisted stretching of any tight muscles around the surgical site.
As soon as possible your physiotherapist will also prescribe strengthening exercises for your knee and lower extremity. These exercises will focus on your quadriceps muscle as well as the muscles of your hip, in particular your gluteal muscles. Gluteal exercises are particularly important, as the hip is the main controller of the position of the knee. The goal of all strengthening exercises will be to regain enough strength and endurance to be able to properly control the alignment of the knee and lower extremity during your everyday and sporting activities. The muscles at the back of your thigh, the hamstrings, as well as your calf muscles, may also require strengthening post surgically. In addition, your therapist may also prescribe exercises for your core area, which also plays a part in maintaining proper alignment of the lower extremities.
After a knee surgery the quadriceps muscle becomes very low in tone and difficult to activate voluntarily, despite no injury to the muscle itself or the nerve that innervates it. This phenomena is termed reflexive inhibition, and it is said to occur in response to several factors including the initial knee injury itself, the swelling in the joint, the reaction of receptors in the knee joint, pain, joint immobilization, and the surgical intervention itself. Reflexive inhibition of the quadriceps muscle after surgery occurs even if you had highly defined thigh muscle tone prior to the surgery. This decrease in tone, if prolonged, will contribute to poor recovery after a knee surgery; therefore exercises to get the quadriceps muscles activated are crucial. It is often noted that the more tone you had prior to the surgery, the quicker the tone returns post surgically. For this reason doing a pre-operative exercise program is highly recommended!
The initial strengthening exercises that your physiotherapist prescribes after an arthroscopic surgery might be as simple as sitting and tightening the quadriceps or buttocks muscles without moving the joint (this type of exercises is termed isometric).
Your therapist may use an electrical muscle stimulator to assist you in contracting the muscles, particularly the quadriceps muscle. As soon as you are able it is important for you to move from the seated position and perform weight-bearing exercises in a functional position, such as standing or squatting. Exercises that work the muscles while in a weight bearing position most effectively assist with daily activities such as walking and stair climbing. Exercises such as squatting, or slowly stepping up or down a step are excellent exercises to encourage the dual activation of both the quadriceps and hamstrings muscles, as well as the muscles of the hip and calf.
Your physiotherapist may again use an electrical muscle stimulator to assist your muscles to contract while you perform these functional exercises. Exercises may also include the use of exercise band, exercise machines, or free weights to provide some added resistance for your thigh and hip. As soon as you are able, and your knee will safely tolerate it, your therapist will advance your exercises to include quicker movements, such as hopping.
They will also encourage more repetitions of each exercise in order to help regain muscle endurance. If you have access to a pool, your physiotherapist may suggest you go to the pool to do your exercises. The buoyancy of the water along with the warmth of the water (provided it is a heated pool) can assist greatly in providing comfort to the knee joint and often allows you to exercise through greater ranges of motion during early rehabilitation.
As a result of any injury or surgery, the receptors in your joints, ligaments, and other tissues that assist with balance and proprioception (the ability to know where your body is without looking at it) decline in function. A period of immobility and reduced weight bearing will add to this decline. If your balance and proprioception has declined, your joints and your limb as a whole will not be as efficient in their functioning and the decline may contribute to further injury in the future. As a final component of our treatment your physiotherapist at In Step Physical Therapy will prescribe exercises for you to regain your balance and proprioception. These exercises might include activities such as standing on one foot or balancing on an unstable surface such as a wobbly board or a soft plastic disc. Advanced exercises will include agility type movements such as hopping on one foot or jumping side to side.
As your range of motion, strength, and proprioception improve, your therapist will advance your exercises to ensure your rehabilitation is progressing as quickly as your body allows. As soon as it is safe to do so, your physiotherapist will add more aggressive exercises such as running, jumping to or from a height, or exercises that mimic the sports and recreational activities that you enjoy participating in. During all of your exercises you therapist will pay particular attention to your technique to ensure that you are not using any compensatory patterns or are developing bad habits in regard to how you use your knee and lower extremity. If you do not pay close attention to how you use your joint and limb post-surgically poor patterns which existed due to pain pre-surgery often continue to occur even once the source of your pain has been eliminated by surgery. The advice from your physiotherapist at In Step Physical Therapy is crucial regarding correcting your movement patterns and developing new, efficient patterns during your daily activities.
Aside from directly rehabilitating the knee after surgery, at In Step Physical Therapy we also highly recommend maintaining the rest of your body’s fitness with regular exercise while your knee is recovering. Cardiovascular exercise can begin very early post-surgically. If you are not yet able to use a normal stationary cycle then an upper body bike can be used instead, or your surgeon may approve of you doing gentle aerobic exercises in a pool as an alternative. A stationary bike, however, is often the best cardiovascular activity once your range of motion and pain levels allow it. Weights for the upper extremities and your other leg are also strongly encouraged. Advanced exercises such as the stepper or elliptical machines may be used once your knee has recovered to an acceptable level. Running is not advised until well into your rehabilitation program as your lower extremity requires both the strength and endurance to tolerate the heavy demands that running puts on the knee joint as well as on the rest of the body. Your physiotherapist at In Step Physical Therapy can provide a program and advice for you to maintain your general fitness while you recover from your surgery.
Usually, the removal of a bipartite patella fragment, fusion of the fragments, or a lateral release are relatively simple surgeries with prompt relief of pain and a quick recovery. Many athletes can expect full range of motion, a stable knee, and a fairly rapid return to normal activity within one to two months with proper rehabilitation. Unfortunately runners and athletes who have had an extended time of immobility, muscle weakness and atrophy, loss of normal joint motion, and patellar tracking problems may require a longer rehabilitation program and a slower return to activity.
When you are well under way with your rehabilitation program, regular visits to In Step Physical Therapy will end. Your therapist will continue to be a resource for you as your recovery continues, but you will be in charge of doing your exercises as part of an ongoing home program.
Generally the rehabilitation after arthroscopic knee surgery responds very well to the physiotherapy we provide at In Step Physical Therapy. If for some reason, however, your pain continues longer than it should, your range of motion is slow to return, or your general therapy is not progressing as your physiotherapist would expect, we will ask you to follow-up with your surgeon to confirm that the knee is tolerating the rehabilitation well and to ensure that there are no complications that may be impeding your recovery.
Portions of this document copyright MMG, LLC
In Step Physical Therapy provides services for physiotherapy in Edmonton.




