Glucosamine and Chondroitin Sulfate for Osteoarthritis of the Knee
|
||||||
Introduction
Physiotherapy in Edmonton for Knee Issues
Welcome to In Step Physical Therapy's guide to Glucosamine and Chondroitin Sulfate for Osteoarthritis of the Knee

Nonsurgical treatment of knee osteoarthritis (OA) focuses on reducing pain and maintaining or improving joint function. Doctors commonly prescribe acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs) to relieve pain and swelling in arthritic patients. Newer NSAIDs called COX-2 inhibitors are showing promise as well.
In recent years, people with knee OA have also been taking two unique compounds. These compounds are gaining greater acceptance among many doctors. Glucosamine and chondroitin sulfate are dietary supplements usually taken in pill form that are thought to protect and possibly help repair cartilage cells.
Glucosamine and chondroitin sulfate are somewhat controversial treatments. While some studies have supported their effectiveness in relieving the symptoms of knee OA, the research still leaves many unanswered questions, especially about long-term effects.
This guide will help you understand:
- what doctors believe the supplements can do
- how the treatments are administered
- what to expect after treatment
- what is In Step Physical Therapy’s approach to rehabilitation
Anatomy
What part of the knee joint does OA affect?
The main problem in knee OA is degeneration of the articular cartilage. Articular cartilage is the smooth lining that covers the ends of bones where they meet to form the joint. The cartilage gives the knee joint freedom of movement by decreasing friction.
The articular cartilage is kept slippery by joint fluid made by the joint lining (the synovial membrane). The fluid, called synovial fluid, is contained in a soft tissue enclosure around synovial joints called the joint capsule.
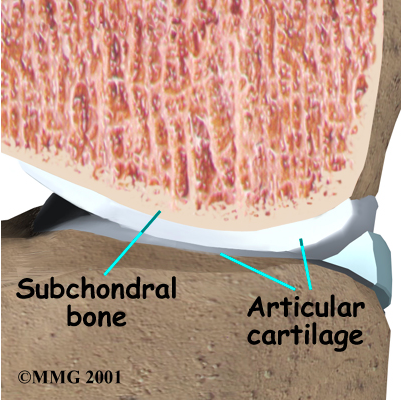
An important substance present in articular cartilage and synovial fluid is called hyaluronic acid. Hyaluronic acid helps joints collect and hold water, improving lubrication and reducing friction. It also acts by allowing cells to move and work within the joint.
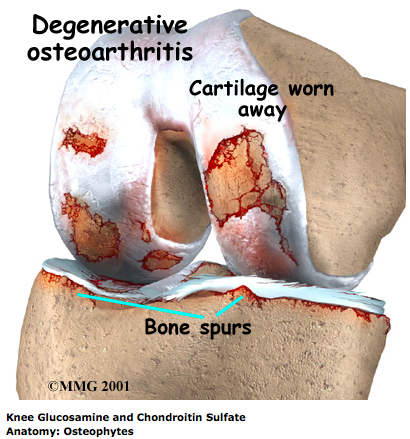
When the articular cartilage degenerates, or wears away, the bone underneath is uncovered and rubs against bone, which causes pain. Small outgrowths called bone spurs, or osteophytes, may form in the joint.
Related Document: In Step Physical Therapy's Guide to Knee Anatomy
Rationale
What do doctors hope to achieve with these compounds?
Glucosamine and chondroitin sulfate occur naturally in the body, mainly in joint cartilage. These substances can also be synthetically made and given in pill form or by injection. The theory is that these supplements can help protect, or possibly even repair, damaged cartilage. Scientific studies lend support to the benefits that these supplements have on reducing pain, swelling, and tenderness, along with improving knee joint mobility.
Laboratory experiments suggest the synovial fluid absorbs glucosamine that is introduced to the body from an external source. Glucosamine supplements also seem to encourage production of hyaluronic acid. Doctors think that normal hyaluronic acid levels in the knee joint keep the cartilage healthy and suppress pain in patients with knee OA.
Glucosamine and chondroitin sulfate also help fight inflammation, which in turn reduces joint pain, swelling, and tenderness from knee OA. These compounds seem to work in a different way than NSAIDs. They take longer to achieve the same benefit, but the results tend to last longer than NSAIDs. Most importantly, they have fewer side effects than NSAIDs. It's possible that some patients may get good pain relief with a combination of the two.
Though the data isn't conclusive, these two supplements have been shown to decrease pain and improve joint mobility in patients with knee OA. In a recent study, knee pain from OA was found to decrease mostly in those people suffering from moderate to severe pain, but not those suffering with just mild pain. Most people start to notice a difference after taking the supplements for four weeks. Maximum benefits happen by eight to 12 weeks, and the benefits seem to last even after treatment has ended. It is usually recommended that glucosamine and chondroitin sulfate can be taken indefinitely as long as one feels that there is relief from symptoms in their affected joints. Long term use (longer than 3 months), however, should be discussed with your doctor to ensure it is safe in each individual case. Studies to support the effectiveness and safe long term use of these supplements are ongoing.
Preparation
How will I prepare for treatment?
It is best to prepare for this treatment by talking to your doctor and gathering any information regarding these supplements for yourself. Organizations in your area that deal with arthritis can be useful (i.e. the Arthritis Foundation of your country.) Not all forms of arthritis respond to these supplements and taking care of knee OA can involve many possible treatments including treatment with physiotherapy. Glucosamine and chondroitin sulfate are not magic bullets. They are one form of treatment in a comprehensive approach to knee OA.
Related Document: In Step Physical Therapy's Guide to Osteoarthritis
Procedure and Complications
How are these treatments administered?
Doctors commonly prescribe oral glucosamine in doses of 500 milligrams three times per day or 1,000 milligrams twice per day. A patient may get a quicker response with a higher dosage. Obese patients may require higher dosages. Most studies of chondroitin sulfate use a dosage of 1,200 milligrams daily.
Complications
What might go wrong?
One potential benefit beyond pain relief for both glucosamine and chondroitin sulfate seems to be that patients experience fewer side effects with these drugs than with NSAIDs.
Most people can take these supplements without complications. Some people, however, complain of gastrointestinal problems, which clear up when patients stop taking the supplement. Although rare, negative reactions may include nausea and vomiting, headache, painful digestion, softened or loose stool, abdominal pain, heartburn, throbbing or fluttering of the heart, skin reaction, edema (swelling), and discomfort in the legs.
Patients who take numerous medications should seek the advice of their doctor before supplementing with glucosamine and chondroitin sulfate. As glucosamine sulfate affects the way insulin works, diabetics are encouraged to monitor their blood glucose levels carefully and to alert their doctor of any marked changes. Also, children, pregnant women, and patients who are on blood thinners should only take chondroitin sulfate with the approval of their doctor.
After Care
What happens after treatment?
Many patients report ongoing benefits, even after they stop taking these supplements. Past studies have shown that the ability of these compounds to fight inflammation may be slower to take effect than NSAIDs yet the benefits seem to outlast NSAIDs. Until further studies are completed it cannot be said that there is proof to show that these supplements rebuild damaged cartilage. Given the possible protection to the cartilage, however, some doctors have their patients use these supplements in hopes of maintaining joint health.
Rehabilitation
Although glucosamine and chondroitin sulfate appear to have a useful place in treating knee OA, it is not recommended they be used alone without any other concurrent treatment. Managing knee OA works best when combined with physiotherapy and lifestyle changes, such as weight loss, and increasing your overall physical fitness.
At In Step Physical Therapy we believe that the more you understand about OA, the more effective our treatment will be. For this reason, we will assist you in learning about OA so you can understand how best to manage your own symptoms.
Regular treatment at In Step Physical Therapy can significantly decrease the pain you feel from your OA knee. The use of heat as well as electrical modalities such as ultrasound or interferential current may be used to alleviate your initial symptoms. Ice may also be a useful depending on individual preference and the stage of the OA. Many patients instead find heat to be particularly soothing on their arthritic joint. Anecdotally, warmer weather often decreases the symptoms of knee OA, whereas cold weather may increase them. This is one reason why many older patients with OA in their joints flock to warmer climates when the colder seasons arrive. Massage to the muscles of the thigh or calf may also be used to aid in pain relief. Acupuncture is gaining popularity as a form of treatment for knee osteoarthritis, and as a result, more studies are being done to validate its effectiveness.
By decreasing the pain you have, it will make it easier for you to do range of motion and strengthening exercises. Knee range of motion often declines as OA progresses so exercises to maintain both the bending and straightening of the knee are important. Your physiotherapist will teach you exercises that you can do in the clinic, as well as part of your home program. Using an exercise bike, whether stationary or regular, is a good way to maintain some of the range of motion of the knee and keep the joint loose. However, because maximum range of motion is not used during cycling, specific exercises that move the knee from full bending to full straightening are still required. There may be a small amount of discomfort as your knee nears the end of the bending or straightening range and this should be respected while still working through your maximum available range. If needed, your physiotherapist will assist you in gaining range of motion by mobilizing the joint. This hands-on technique helps to encourage the knee joint to move gradually into the end ranges of motion.
In addition to range of motion exercises, your physiotherapist will teach you strengthening exercises for the knee and hip. The hip is particularly important as it controls the alignment of the knee so weakness in this area in particular leads to undue forces being put through the knee during everyday activities such as walking or stepping up or down. OA can affect both sides of the knee joint but in many cases the knee cartilage wears down on one side (typically the medial or inside of your knee) quicker than the other side, which then significantly affects the alignment of your knee. Your physiotherapist may use an electrical muscle stimulator on the muscles around the knee or hip to encourage the muscles in these areas to fire, which supports your joints, improves your alignment, and therefore takes the pressure off of your painful knee. Light weights or elastic bands may also be used to add increased resistance and build up the strength.
Alignment can also be improved by implements such as wedged foot orthotics or knee braces. Wedged orthotics change the ground forces that are applied upwards to your knee and specialized knee braces are designed to unload the pressure off of the most painful side of your knee. Another way to unload the pressure on your knee is to use a cane or walking stick. Research has shown that the use of a cane in the hand that is opposite to your painful knee will decrease the forces applied to your knee and may therefore decrease your pain. On that note, if you are carrying heavy goods, carrying them on the same side as your OA knee instead of in the opposite hand will put the least amount of pressure on your painful joint. Your physiotherapist at In Step Physical Therapy will assess your knee and determine if your knee would benefit from the use of orthotics, a brace, or a walking aid, and will refer you to the appropriate health care professionals to assist you with obtaining these items.
If you are overweight, losing some weight can also take pressure off of your painful knee. Any extra weight that the body carries will put direct pressure on your OA knee and increase the amount of pain you feel and hasten the process of joint deterioration.
Your physiotherapist will encourage weight loss through both dietary changes as well as strength training, and cardiovascular activities such as walking (if tolerable), stationary or ordinary cycling, or pool activities such as swimming or water aerobics. The pool is a particularly good venue to partake in cardiovascular activities for weight loss as well as perform many of the exercises your physiotherapist prescribes for range of motion and strengthening. The water naturally takes some of the pressure off of your joint and therefore many patients with OA find the water particularly therapeutic especially if the water is warmer than usual public pool temperature.
The final part of our treatment will include exercises for your balance. As the result of any injury or pain the receptors in your joints and ligaments that assist with balance and proprioception (the ability to know where your body is without looking at it) decline in function. This is true with OA knees as well. Your physiotherapist at In Step Physical Therapy will prescribe exercises for you to regain and maintain this balance and proprioception. This might include exercises such as standing on one foot or balancing with both feet on an unstable surface such as a pillow or a soft plastic disc. Depending on the stage of your OA and your ability, your physiotherapist may even prescribe agility exercises such as gentle hopping or moving side to side.
Fortunately, most patients with knee OA who combine the use of glucosamine and chondroitin sulfate with our rehabilitation program at In Step Physical Therapy feel that their pain decreases, they are better able to manage their symptoms, and are also able to improve their activity level and quality of life. If, however, your knee does not respond as we would expect to the treatment we provide at In Step Physical Therapy, we will promptly liaise with your doctor regarding the best management plan to assist you.
In Step Physical Therapy provides services for physiotherapy in Edmonton.
Portions of this document copyright MMG, LLC.




